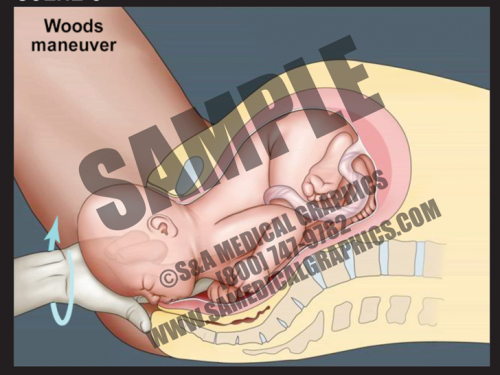
- This 2D dissolve animation shows how this maneuver can release shoulder dystocia impaction and allow for delivery of the fetal shoulder.
- Each animation has pause and play buttons to allow for more interactivity during viewing.
-
-
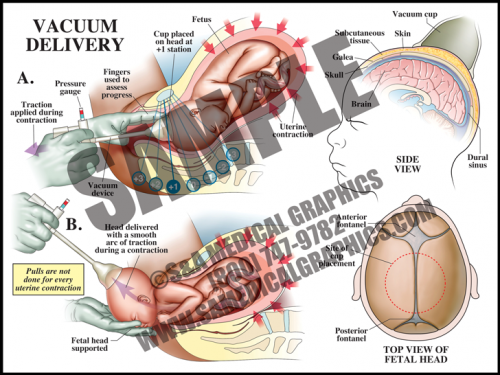
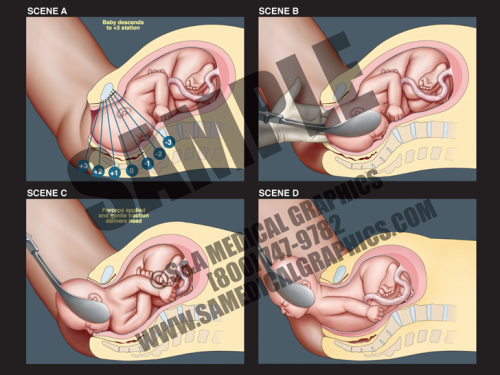
- Vacuum delivery may be performed in cases where there is a prolonged second stage of labor or suspicion of immediate or potential fetal compromise. This procedure assists delivery by helping to move the baby through the birth canal.
- The vacuum cap is a simple device that is placed on the vertex of the head with a small hand-held vacuum pump; some physicians leave the vacuum on between contractions and some release the vacuum. The caps are set to pop off if the vacuum pressure is too high.
- This procedure works with the uterine contractions, gently assisting and guiding the fetus out during contractions, and resting between them. It is not used between contractions.
-
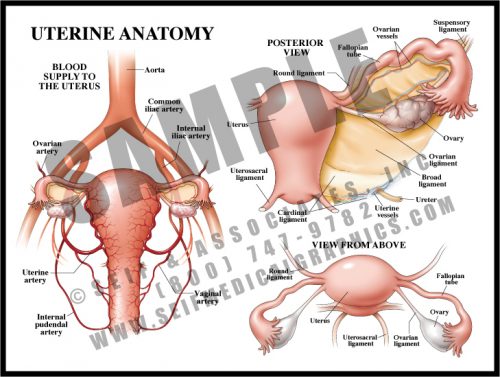
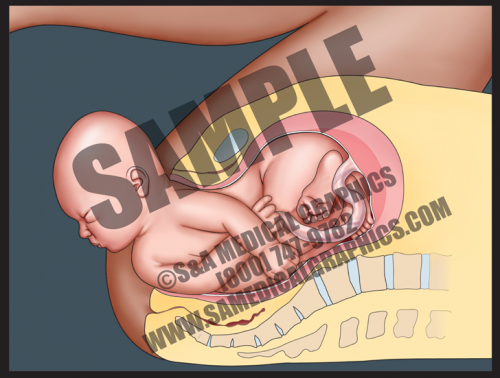
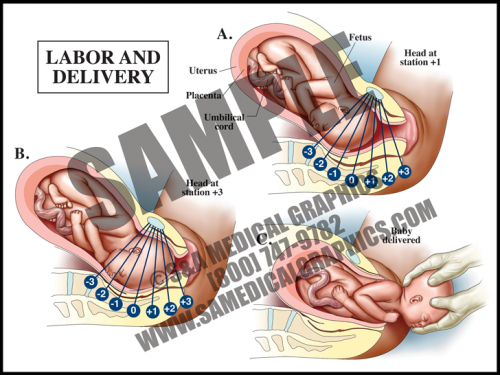
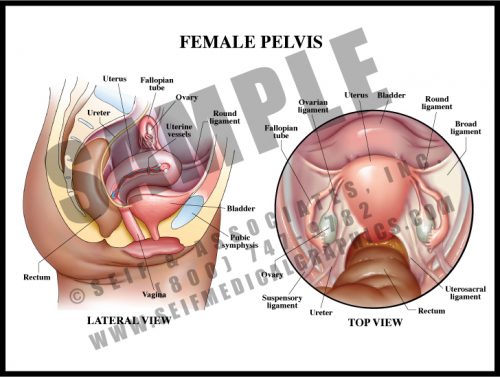
- The uterus is small and contracted in its non-pregnant state, but grows to fill nearly the entire abdomen during pregnancy. Delivery is effected by repeated strong contractions pushing the fetus through the cervix and out the birth canal (vagina).
- The fallopian tubes carry the ova to the uterine cavity, where fertilized eggs implant and develop.
- The blood supply to the uterus is redundant and increases greatly during pregnancy.
-
- This 2D dissolve animation shows how this maneuver can release shoulder dystocia impaction and allow for delivery of the fetal shoulder.
- Each animation has pause and play buttons to allow for more interactivity during viewing.
-
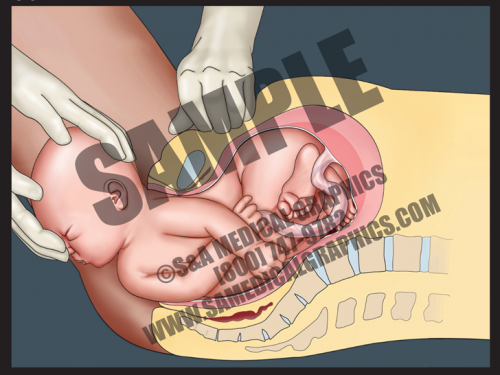
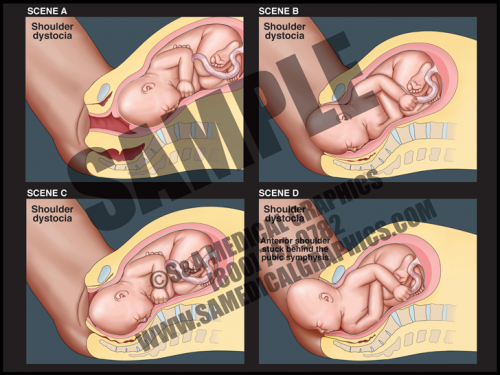
- This 2D animation demonstrates how shoulder dystocia occurs during delivery.
- It shows fetal descent down the birth canal and delivery of the fetal head, but impaction of the anterior shoulder on the pubic symphysis, preventing delivery of the shoulder.
- This animation has pause and play buttons to allow for more interactivity during viewing.
-
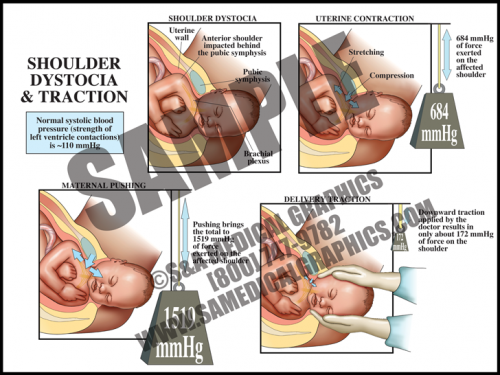
- The uterus itself generates tremendous pressure during contractions. If the average systolic blood pressure (pressure generated by the left ventricle during a contraction) is 120 mmHg, the uterus alone generates more than 5 times that amount. When the accessory muscles (the diaphragm and abdominal muscles) are used to push in conjunction with contractions, this pressure increases to more than 10 times that amount.
- The pull generated by a physician during downward traction for shoulder dystocia is slightly higher than the average systolic blood pressure and contributes only a very small amount to the total amount of generated pressures.
- Uterine and abdominal pressures are good evidence that if shoulder dystocia is the cause of brachial plexus palsy, it is most likely from the intrinsic pressures of the uterus and body wall, not the caregiver.
-
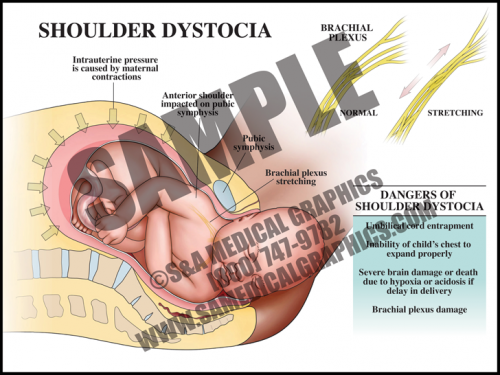
- In cases of shoulder dystocia, the upper fetal shoulder is impacted on the pubic symphysis, or more rarely, the lower shoulder becomes impacted on the sacral promontory or nonexible coccyx. In either case, this event prevents delivery of the baby. Shoulder dystocia can be a potentially catastrophic event since the fetal thorax is still within the pelvis and cannot properly expand for breathing.
- While the rate of shoulder dystocia is higher with gestational diabetic women and macrosomic fetuses (>4500 grams at birth), most cases of shoulder dystocia occur with average-sized fetuses.
- If a brachial plexus palsy (brachioplexopathy) occurs, it usually affects the portions of the brachial plexus that control the shoulder and elbow. Spontaneous recovery is the rule rather than the exception.
- Most fetuses are successfully delivered with a combination of McRoberts maneuver and suprapubic pressure.
-
- This 2D dissolve animation shows how this maneuver can release shoulder dystocia impaction and allow for delivery of the fetal shoulder.
- Each animation has pause and play buttons to allow for more interactivity during viewing.
-
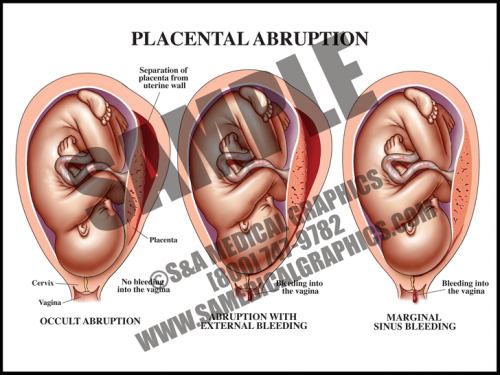
- Abruption occurs when the placenta separates from the uterine wall. Most of the time, this is accompanied by vaginal bleeding as the blood travels between the membranes and the uterus. Some- times, however, there is no bleeding because edges of the placenta remain sealed.
- Symptoms frequently include hypertonic uterus with severe abdominal pain and rapid contractions. If the abruption is large (more than about 50%), the fetus may not survive.
- The specific cause of placental abruption is often unknown, but risk factors include abdominal trauma and maternal factors like smoking, drinking, and diabetes, among others.
- Fetal distress occurs early in this condition in about half of all cases.
-
- This 2D animation demonstrates the nor- mal course of labor, showing the dilation of the cervix, descent of the fetus, delivery of the fetal head, and finally delivery of the fetal shoulders and body.
- This animation has pause and play buttons to allow for more interactivity during viewing.
-
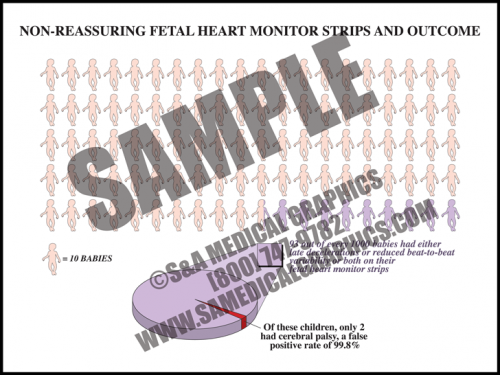
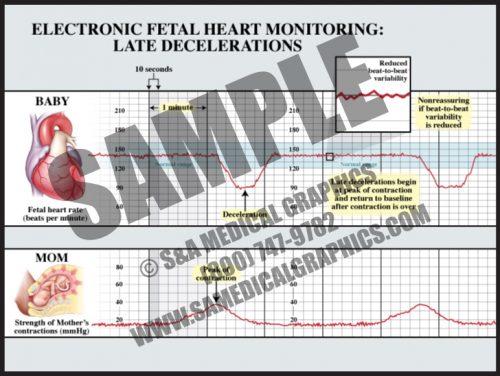
- One risk of fetal heart monitoring technology is false-positive results.
- In fact, “nonreassuring” FHM strips, or those which show either late decelerations, or reduced beat-to-beat variability, or both, have a greater than 99% false-positive rate in predicting cerebral palsy.
-
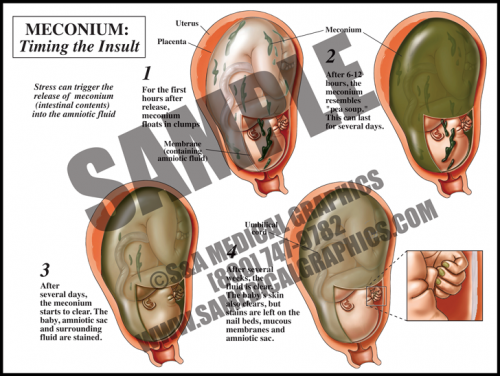
- Meconium is the dark, tarry contents of the fetal gastrointestinal tract. Meconium passage at labor and delivery is common and not a sign of fetal distress unless it is accompanied by other ominous signs.
- Meconium release into the amniotic fluid is however considered a sign of intrauterine fetal distress. This can be caused by placental insufficiency, maternal hypertension, and preeclampsia, among other things.
- When meconium is freshly released, it is clumpy and oats in the amniotic fluid. Within hours, it distributes particulate matter throughout the sac. Macrophages in the fetal skin, mucus membranes, and the amniotic sac phagocytize the particles, giving a green cast to the tissues.
- After several days, the fluid is greenish-brown but clear, and the fetus and membranes are stained. After several weeks, the fetal skin and fluid will clear, but the amniotic membranes, fetal mucus membranes, and nail beds remain stained.
-
- This 2D dissolve animation shows how this maneuver can release shoulder dystocia impaction and allow for delivery of the fetal shoulder.
- Each animation has pause and play buttons to allow for more interactivity during viewing.
-
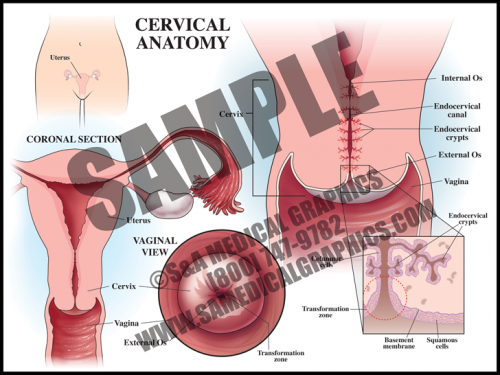
- In the first stage of labor, the cervix must thin (efface) and open (dilate) to a diameter of about 10 cm (4 in) in order to allow the fetal head to pass through.
- Repeated uterine contractions pushing the fetal presenting part against the inside of the uterus cause the cervix to thin and open over time.
- The fetal presenting part is considered to be engaged when the lowest portion is at the level of the ischial spines; this is called the 0 station. Fetal movement down the birth canal is measured by positive stations, using a 0/+3 scale or a 0/+5 scale.
- The second stage of labor starts at full dilation of the cervix and is completed when the fetus is delivered. The third stage is the delivery of the placenta.
-
- Forceps delivery is a type of operative vaginal delivery performed to help guide the baby out of the birth canal if the second stage of labor isn’t progressing or if fetal safety depends on immediate delivery.
- This 2D animation shows how this procedure is performed, showing that once the fetus has descended far enough down the birth canal, a health care provider applies the forceps to the fetal head.
- The forceps are then used to gently assist and guide the fetus out of the birth canal during uterine contractions. Forceps are not used between contractions.
-
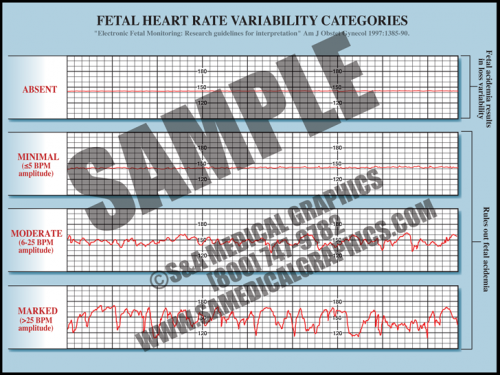
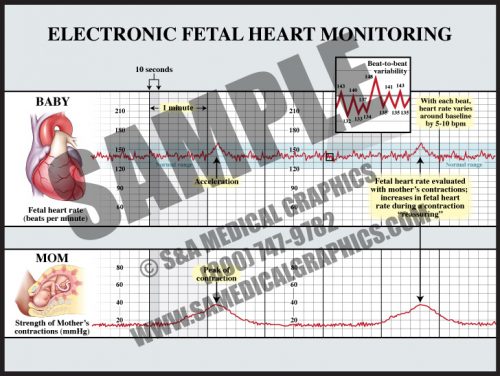
- Fetal heart rate is constantly varying from the baseline; this variability reflects a healthy fetal nervous system and cardiac responsiveness.
- These fluctuations are characterized as absent if there is no variation in the amplitude range, minimal if fluctuation is less than 5 bpm, moderate if fluctuation is 6 to 25 bpm, and marked if fluctuation is greater than 25 bpm.
- Absent variability indicates fetal academia but marked, moderate, and even minimal variation rules it out.
- Conditions like fetal hypoxia, congenital heart anomalies, and fetal tachycardia can cause a decrease in variability.
-
- The female pelvis contains the bladder, uterus, vagina, and rectum. The tissue between the vaginal and rectal openings is a tight collection of tendons from the pelvic floor muscles, the perineum. The entire region is called the vulva.
- The non-pregnant uterus is about the size of a small pear. It is a hollow muscular organ, its neck enclosed by a thick circular muscle known as the cervix.
- Urine is excreted from the kidneys via the ureters, which transport it to the bladder. It is then carried to the outside by the relatively short urethra.
- The ovaries release ova (eggs) each month to the uterus via the fallopian tubes; ovarian hormones are absorbed into the bloodstream.
- The organs are held in the pelvis by a number of ligaments connecting them to the pelvic walls.
-
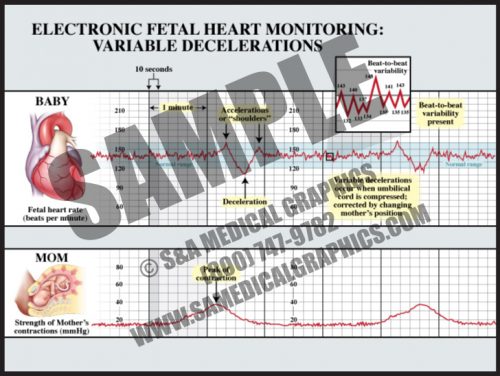
- Variable decelerations can occur at any time during or between contractions and are usually characterized by “shoulders” before and sometimes after the deceleration.
- The decelerations are usually “V” or “U”-shaped and return to baseline within two minutes or less.
- Variable decelerations are due to head or cord compression and are “treated” by changing the mother’s position and applying oxygen.
- Unless very deep (<60 bpm) for extended periods (>2 minutes or more), they are considered benign.
- Variable decelerations occur during the second stage of most labors, as the fetal head moves down the narrow vaginal canal and is compressed by a combination of the uterine contractions and the narrow vagina.
-
- This technology, used in approximately 87% of all labors in the U.S., tracks the fetal heart function against uterine contractions.
- The normal fetal heart rate is approximately 120-160 beats per minute (bpm), although normal individual fetuses might be higher or lower than this range.
- Beat-to-beat variability is literally the changes of the fetal heart rate from beat to beat (short-term variability), and within 3-5 minute periods (long-term variability). Beat-to-beat variability decreases or disappears for 20-30 minute time periods as the fetus sleeps, but is present in most normal labors and represents the health of the fetal brainstem.
-
- Late decelerations start at or after the peak of a contraction and are considered to be a sign of uteroplacental insufficiency.
- The depth of late decelerations is probably not as significant as their presence. If frequent, they can be a sign of fetal distress and an indication for prompt delivery.
- If late decelerations are accompanied by loss of beat-to-beat variability, it is generally considered an indication for urgent or emergent delivery, either by cesarean section or operative delivery (forceps or vacuum extraction), depending upon the state of the labor.
- The vast majority of fetuses with nonreassuring fetal heart tracings are completely normal.
-
- The cervix is the circular muscle at the base of the uterus; it makes up the top of the vagina.
- The cervical canal passes through the cervix and allows blood from menstruation and a fetus to pass from the uterus into the vagina.
- During a pap smear, a screening test for cervical cancer, cells are scraped from the opening of the cervix and examined under a microscope for abnormality.
- The transformation zone is the area where the mucus secreting columnar cells of the endocervix meet the squamous cells of the ectocervix. Most squamous cell carcinomas and dysplasias are found here.
-
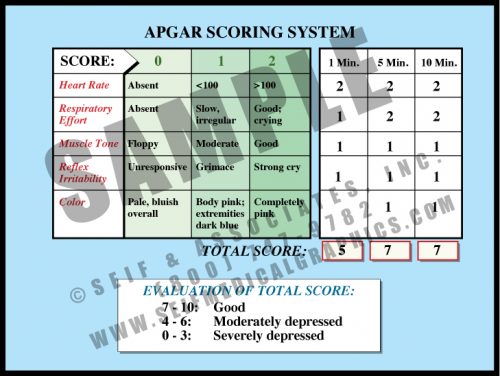
- This simple scoring system indicates how well the fetus fared through labor and delivery. The maximum score is 10 and the minimum is 0, with up to 2 points being awarded for each of 5 measures of health.
- Apgar scoring is done at 1 minute and 5 minutes of age, sometimes by nursing staff, sometimes by physicians. If the 5-minute score is low, a 10, 15 or 20-minute score may be recorded, either until the baby is stable or moved from the delivery room for specialized care.
- While there is some correlation between low 5 minute Apgar scores and neurological outcome, only a very small percentage of children with low 5 minute scores sustain brain damage. The longer the score remains low, the higher the correlation with neurological damage.
-
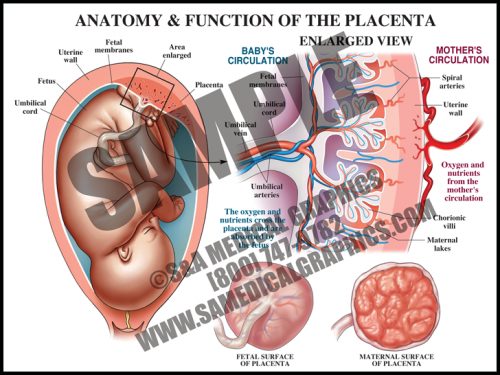
- The placental is a flattened, circular organ that develops in the uterus during pregnancy in order to support the fetus. The fetus is attached to the placenta via the umbilical cord.
- The placenta transfers oxygen and nutrients from the maternal blood to the fetal blood; it also transfers wastes products from the fetal blood to the maternal blood for removal.
- The umbilical cord is normally comprised of three blood vessels, two smaller umbilical arteries that carry deoxygenated blood from the fetus to the placenta, and a larger umbilical vein that supplies the fetus with oxygenated blood from the mother.
- The placenta is expelled from the uterus after the fetus is delivered. Placental pathology can reveal important information about intrauterine conditions and events, as well as shed light on the cause of adverse fetal outcome.
-
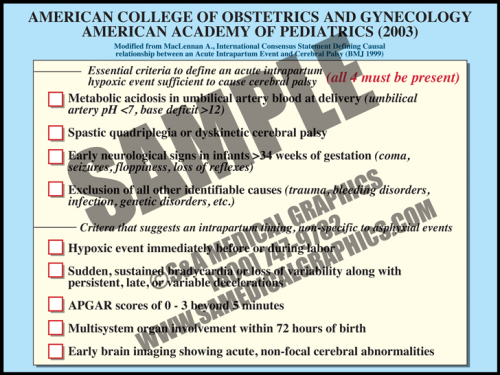
- In 2003, the American College of Obstetrics and Gynecology and the American Academy of Pediatrics recommended adoption of a definition of term intrapartum asphyxia developed by an international task force.
- The definition requires that all four parameters must be met in order to diagnose intrapartum asphyxiation in a term fetus. These include metabolic acidosis, diagnosis of specific types of cerebral palsy correlated with the types of asphyxia damage seen in term fetal brains, early seizures and other neurological signs, and exclusion of all other causes.
- There are other criteria that suggest an intrapartum timing of injury, nonspecific to asphyxia event. These include a hypoxic event immediately before or during birth, sudden, sustained bradycardia or loss of variability along with persistent, late, or variable decelerations, low APGAR scores (<3) beyond 5 minutes, multisystem organ involvement within 72 hours of birth, and early brain imaging showing acute, non-focal cerebral abnormalities.