This case involved an obese male patient with a multi-year history of lower leg pain and numbness. He eventually underwent decompression and fixation of the thoracic spine. After the procedure, he experienced pain relief but was unable to move his legs. A CT showed one of the pedicle screws to be somewhat medially positioned although not enough to cause paralysis. Still, a revision surgery was performed to correct the screw position. During surgery it was observed there was no impingement whatsoever of the thecal sac but the screw was re-positioned to a more lateral position. Unfortunately, the patient did not regain motor function.
The plaintiff alleged the misplaced pedicle screw damaged the spinal cord causing loss of motor function. The defense contended the plaintiff was neurologically compromised from his extensive multilevel disease and that he had actually been experiencing intermittent paralysis and cauda equina symptoms for many years. Further, during the hardware revision surgery, the surgeon visualized no impingement of the spinal cord at all. The medical team provided excellent care during this extremely difficult case, which was complicated by obesity and several co-morbidities. Unfortunately, failure to regain motor function is not an unexpected outcome for a patient with a history of years of severe spinal stenosis.
The plaintiff alleged the misplaced pedicle screw damaged the spinal cord causing loss of motor function.
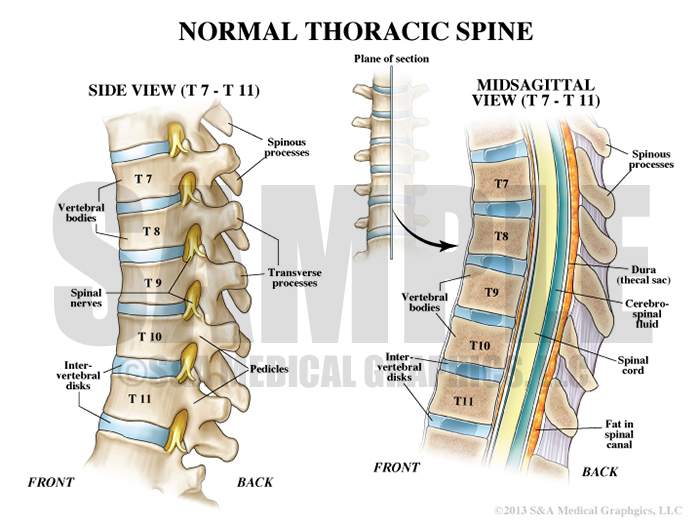
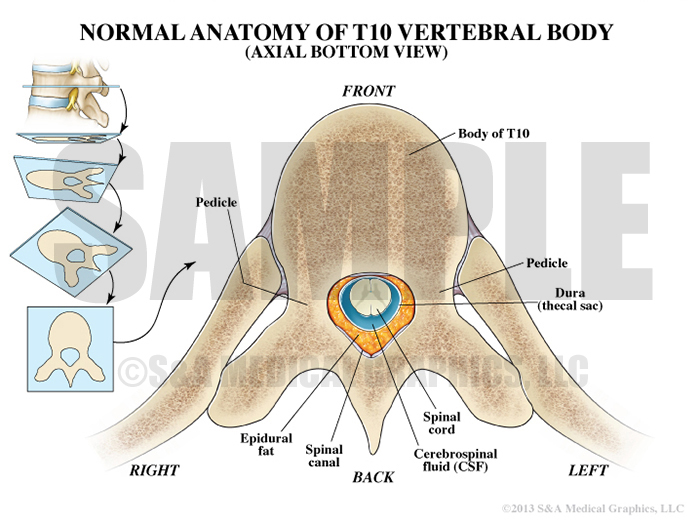
The defense’s first visual goal was educate the jury on the normal anatomy of the thoracic spine focusing specifically on the anatomy of the spinal cord and spinal nerves. Orientation images and different anatomical views were used to explain this complex anatomy and introduce the imagery that would become critical in later exhibits. By teaching the jury the normal anatomy, the defense team was able to compare and contrast the severe pathology observed in this case.
Exhibit 1 depicts normal thoracic spine anatomy.
Exhibit 2 depicts normal T10 vertebral body anatomy.
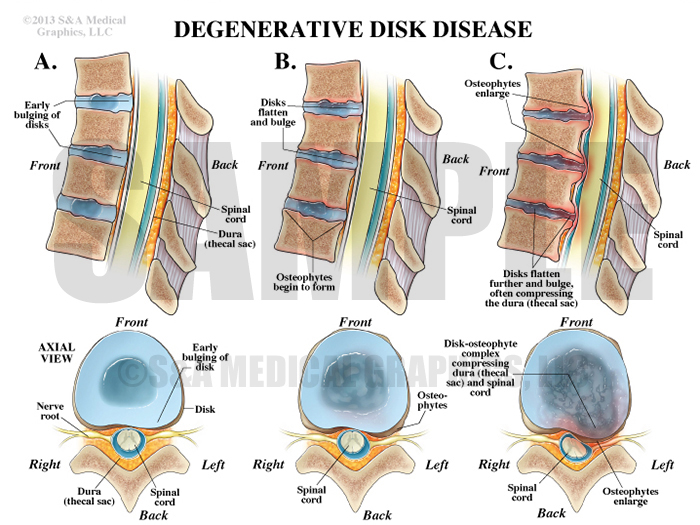
Once normal anatomy of the thoracic spine had been defined, the concept of degenerative disk disease was introduced visually. This exhibit was designed to help the jury understand this condition and why it results in pain. It was used alongside patient specific exhibits to allow the jury to clearly see and identify the pre-operative disease found in this patient.
Exhibit 3 depicts steps of degenerative disk disease.
Exhibit 4 depicts the spread of cancer.
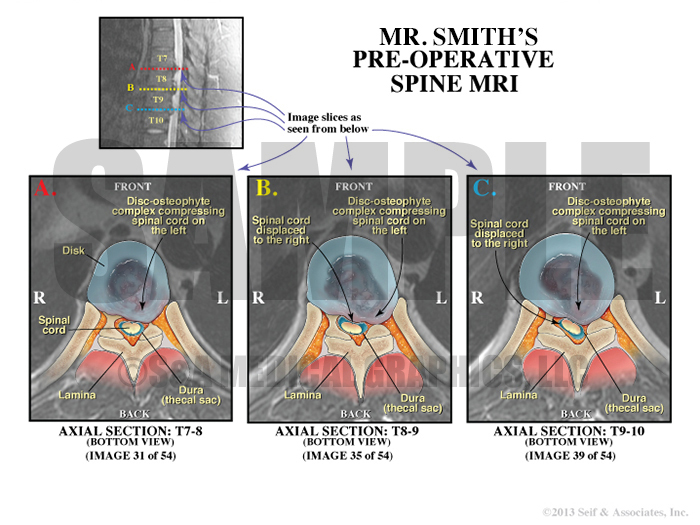
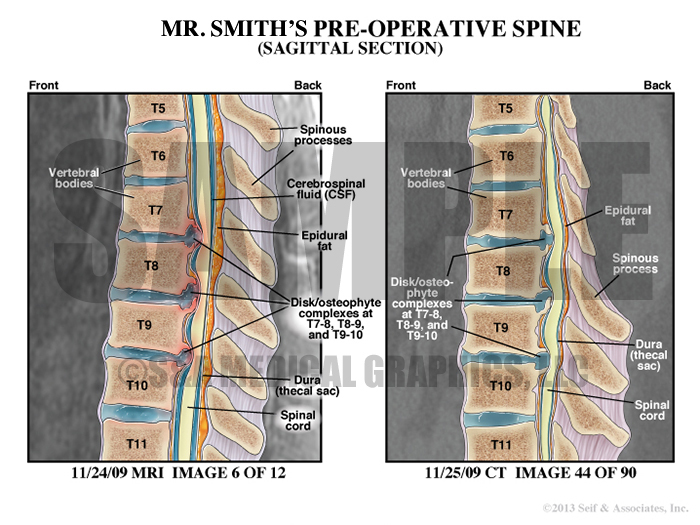
Exhibit 5 explains patient’s preoperative condition.
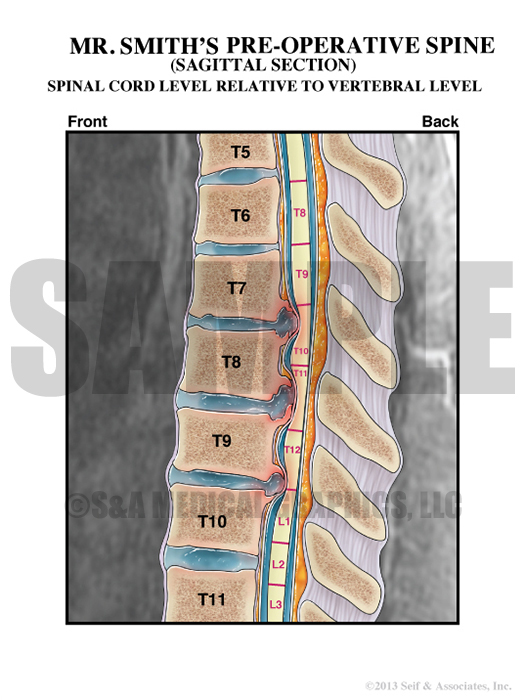
Exhibit 6 depicts spinal cord level relative to vertebral level.
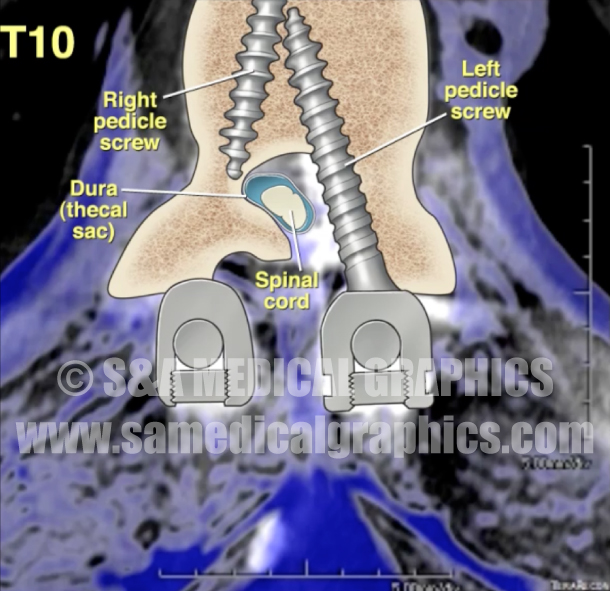
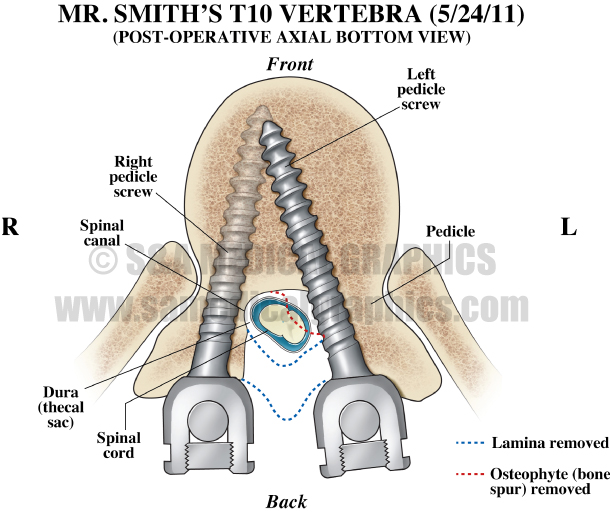
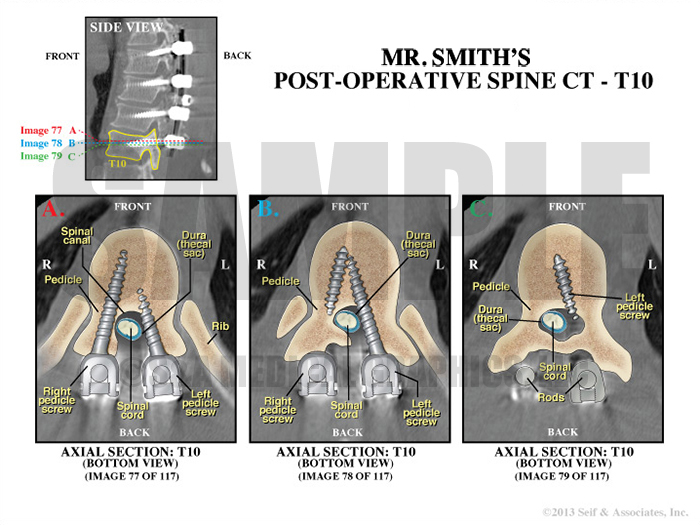
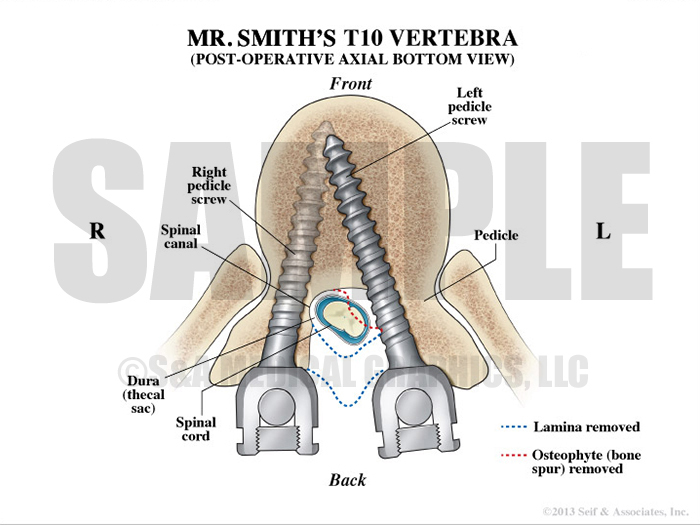
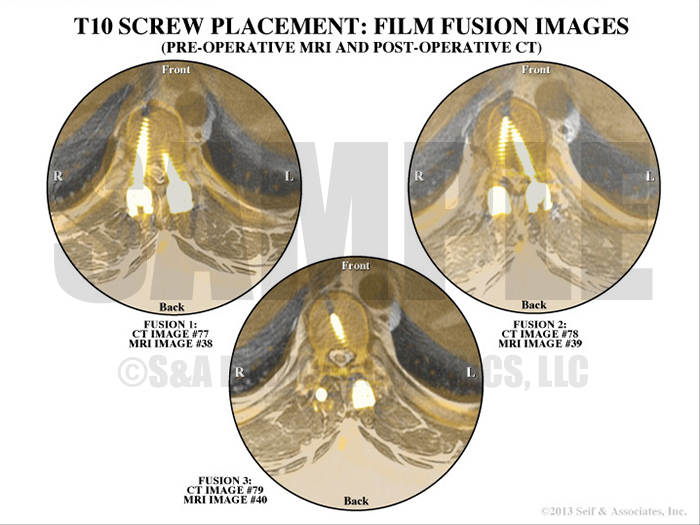
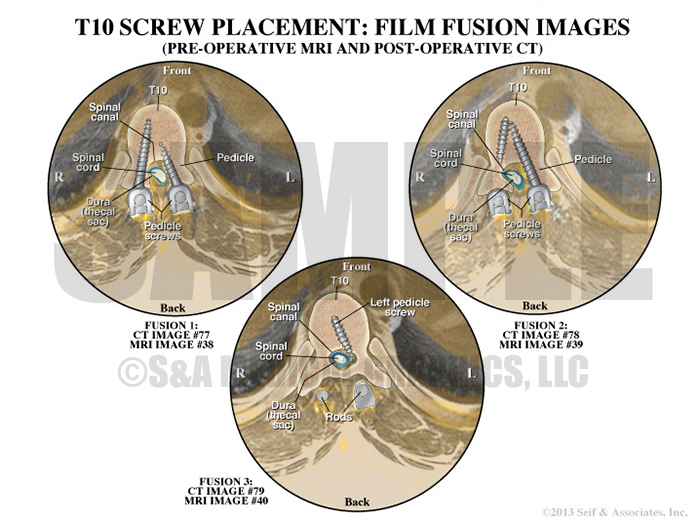
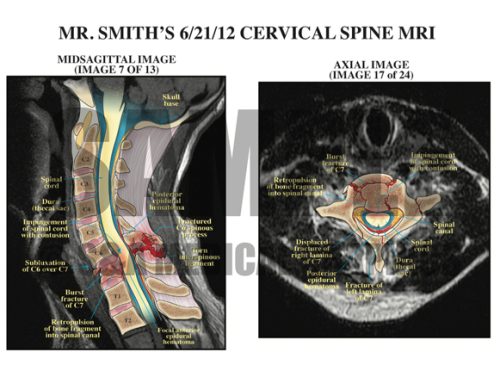
In order to counter the plaintiff’s allegation that the pedicle screw damaged the spinal cord, we created an exhibit to illustrate what was seen on the patient’s post-operative MRI and CT studies. We worked closely with the expert neuroradiologist in order to create exhibits that highlighted the fact that the thecal sac was not impinged whatsoever, therefore making clear it was highly unlikely the pedicle screw placement caused this patient’s paralysis.
Exhibit 7 depicts the patient’s postoperative spine.
Exhibit 8 depicts pedicle screw positions in patient’s T10 vertebra.
Exhibit 9 visualizes the patient’s preoperative MRI and postoperative CT overlapped.
Overlay interpretation of pedicle screws and rods.
To further emphasize the crucial 3D anatomical relationships in this case, we created a reconstruction of the CT studies. This video was combined with illustrations to help the jury see where the spinal hardware was placed.
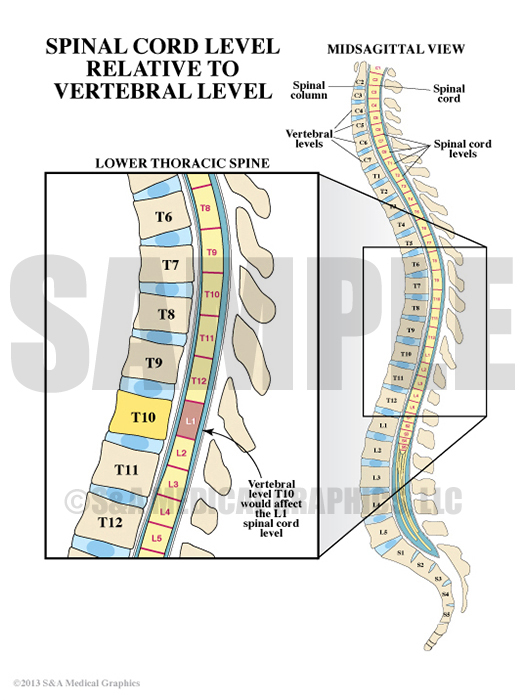
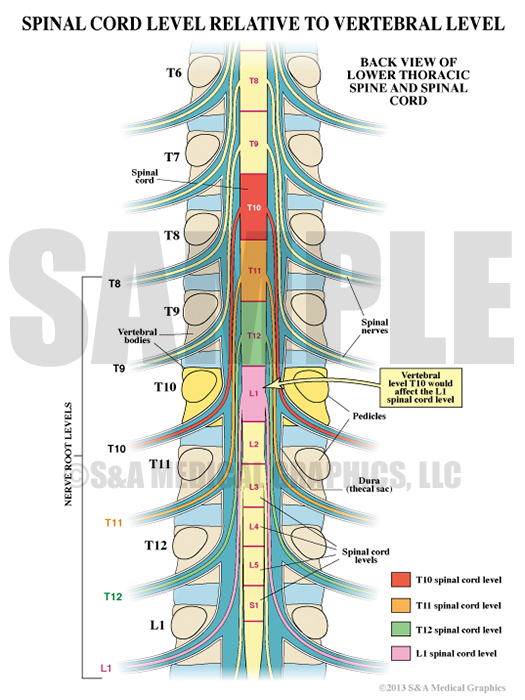
To further emphasize the alleged malpositioned screw could not have caused the patient’s symptoms, two exhibits were created to illustrate the difference between vertebral level and myelomere level. They show that an injury at the T10 vertebral level would actually affect the spinal cord at a much lower functional level resulting in a pattern of dysfunction very different from an injury to the cord at T10. Ultimately, these 2 exhibits were used to help show that this patient’s pattern of dysfunction did not correspond to an L1 cord level injury – as expected with a T10 vertebral injury.
Exhibit 10 explains a vertebral level T10 would affect the L1 spinal cord level.
Exhibit 11 depicts the different spinal cord levels.
—Editorial contributed by Emily Ullo Steigler, MS, CMI
—Illustrations contributed by Robert Edwards, MS, CMI