This case involved a 19-year-old male patient who had a history of low back pain for about a year and was reporting severe, constant, and aching lower back pain of 8-9 on a scale of 10, as well as radicular right leg pain, decreased sensation on the right, difficulty straightening his right leg making it difficult to walk. An MRI showed a rather large L5-S1 herniated disk on the right side with severe degenerative disk disease.
The defendant performed an L5-S1 decompression with posterior lumbar interbody fusion and placement of a TraXis cage. Infuse and autograft were used to complete the interbody fusion. Intraoperatively, the defendant found that the patient had severe degenerative disk disease with a large right paracentral disk herniation, with the disk acting like a broad-based disk bulge with some components of hard and soft disk. There were no significant sequestered or extruded fragments, however.
Postoperatively, the patient initially reported an improvement in his leg pain and less discomfort in his lower back. Within a month, however, he was complaining of significant ongoing pain and was also displaying significant narcotic seeking behavior. The defendant began tapering the patient’s narcotics and prescribed him physical therapy. The patient continued to complain of rather significant lower back pain, however. A diagnostic x-ray showed that the grafts and hardware were in good position, although a CT myelogram done three months later did show some ectopic bone formation in the spinal canal in the area of the diskectomy, but the nerve root appeared to be above the level of the bony spur. The patient continued to complain of back pain and diagnostic studies continued to show no evidence of disk herniation or nerve root impingement and an EMG showed normal sensory nerve conduction.
The plaintiff alleged that the BMP that the defendant used during surgery caused ectopic bone growth and that this bone growth pushed on the nerve roots, causing the plaintiff’s continued lower back and leg pain. The defense contended that the ectopic bone growth was not pushing on the nerve and that the pain the plaintiff was experiencing was from his previous pathology.
The plaintiff alleged that the BMP that the defendant used during surgery caused ectopic bone growth and that this bone growth pushed on the nerve roots, causing the plaintiff’s continued lower back and leg pain.
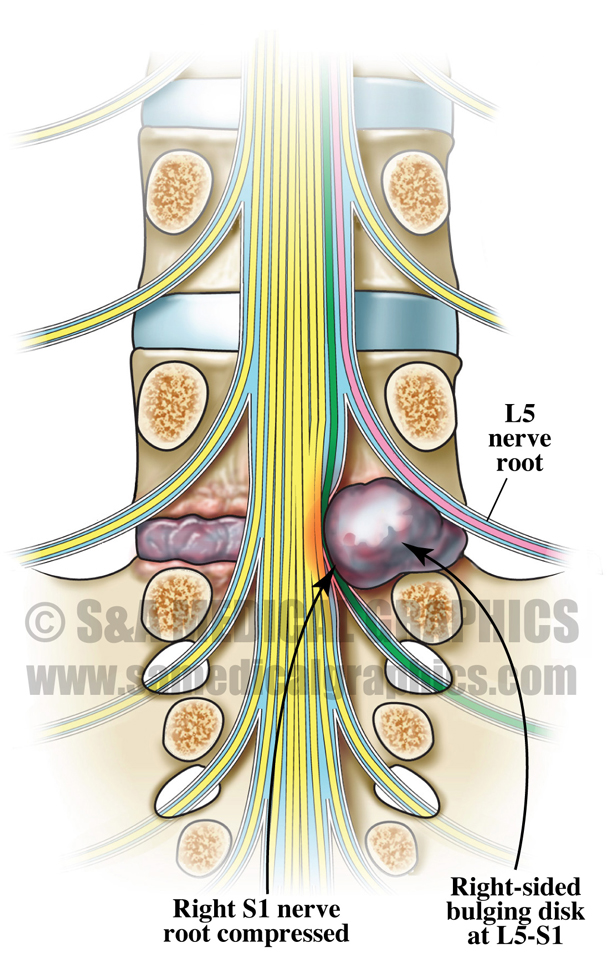
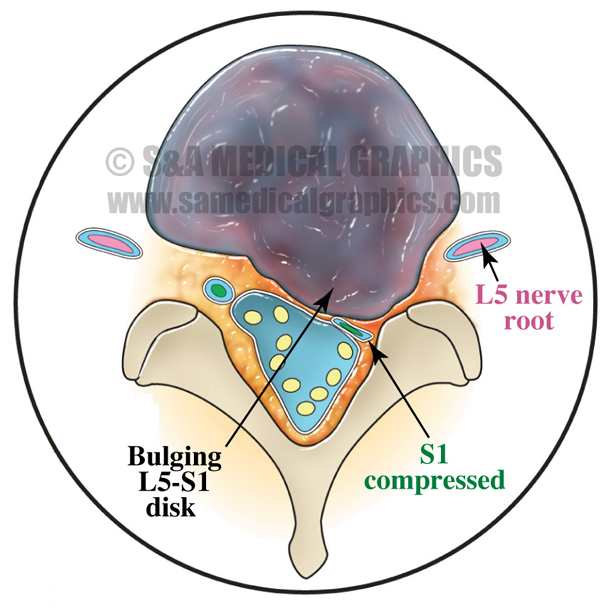
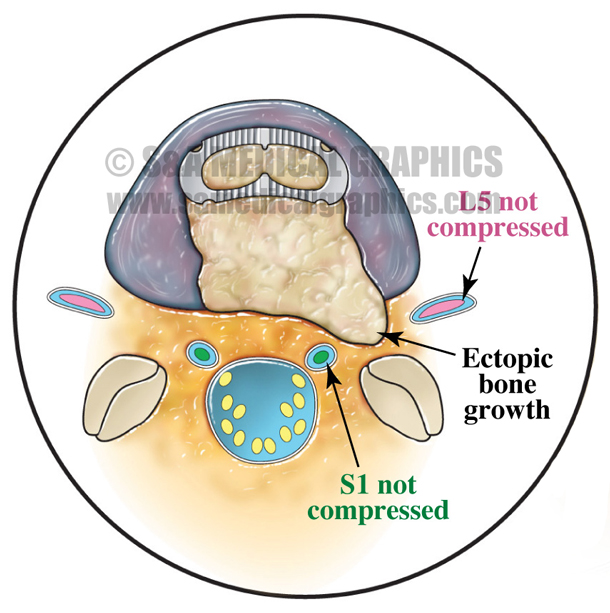
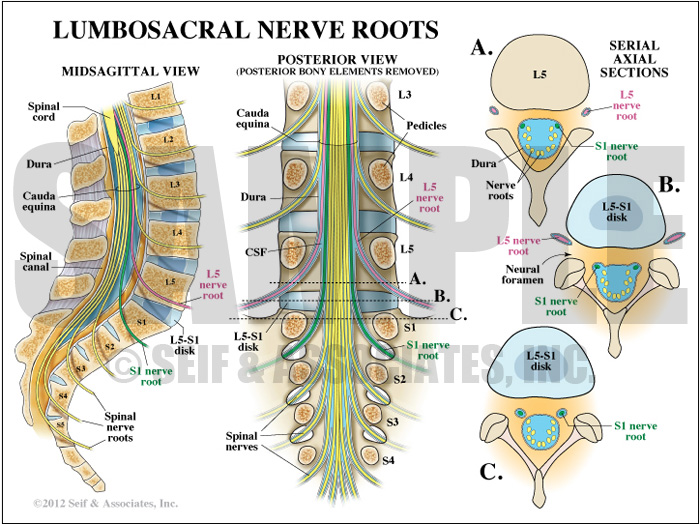
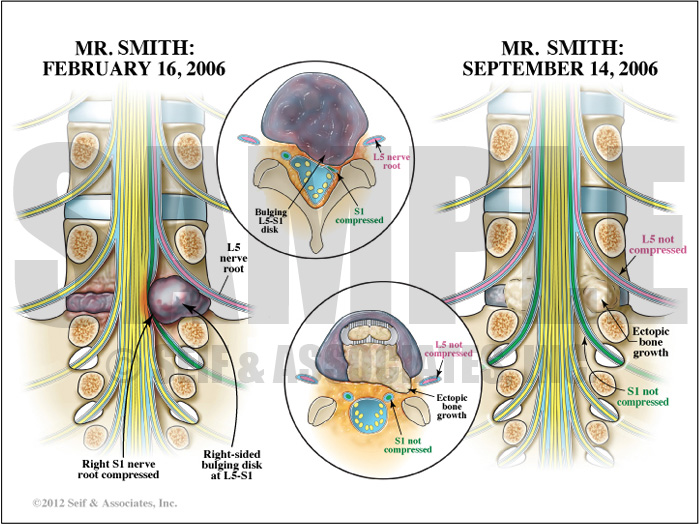
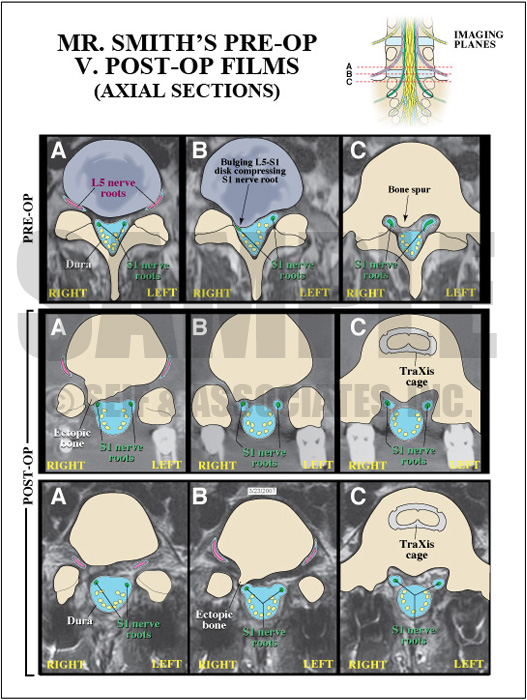
The first goal of the defense visual strategy was to allow the jury to see the normal anatomy of the lumbosacral nerve roots and to show how they exit the foramen at L5-S1. This could then be used in conjunction with a second board for comparison against the plaintiff’s preoperative and postoperative anatomy, in order to show how his nerve roots exited at that level before and after the defendant’s procedure. These exhibits were designed for side-by-side use in order to clearly show that preoperatively the plaintiff’s S1 nerve root was compressed by his bulging L5-S1 disk; the L5 nerve root was not directly compressed. Postoperatively however, both the S1 and L5 nerve roots were decompressed and remained so, unaffected by the ectopic bone growth in the spinal canal, with the L5 nerve root exiting above the growth and the S1 nerve root exiting below the growth. Color-coding of the L4 and L5 nerve roots helped to focus the jury’s attention on the path of these 2 pairs of nerves.
Exhibit 1 depicts the location of lumbosacral nerve roots.
Exhibit 2 depicts the patient’s nerve root compressed by bulging disk.
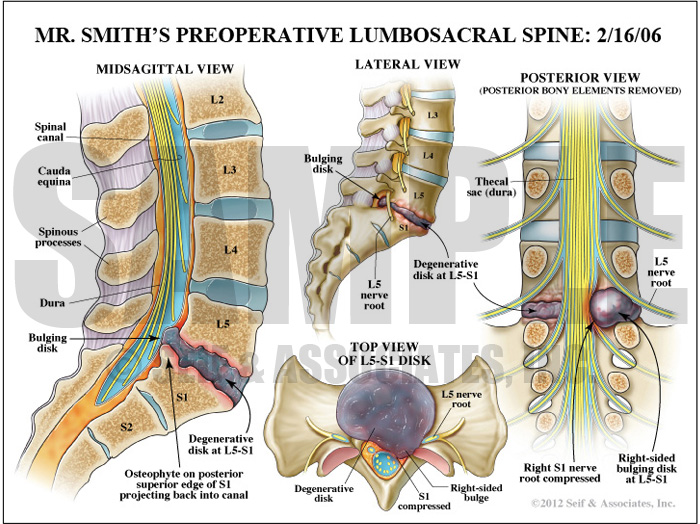
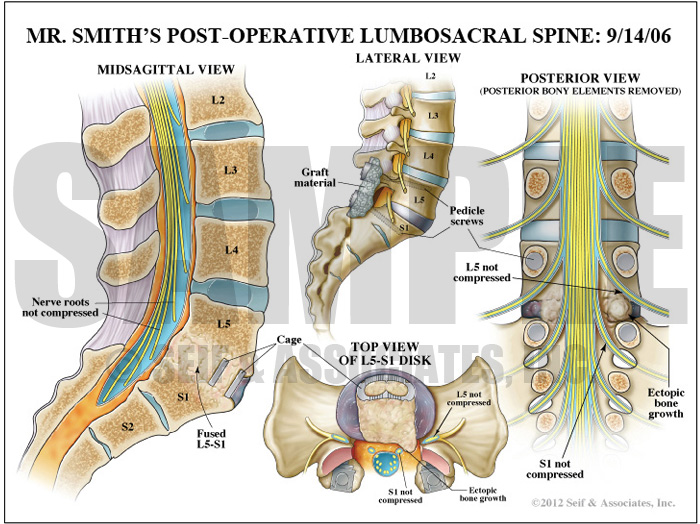
The next exhibit went in to further detail to show the preoperative condition of the plaintiff’s lumbosacral spine, showing his large disk herniation and severe degenerative disk disease, as well as the postoperative condition of the plaintiff’s lumbosacral spine, showing the decompression and benign ectopic bone growth.
Exhibit 3 depicts the patient’s preoperative spine anatomy.
Exhibit 4 depicts the patient’s postoperative spine anatomy.
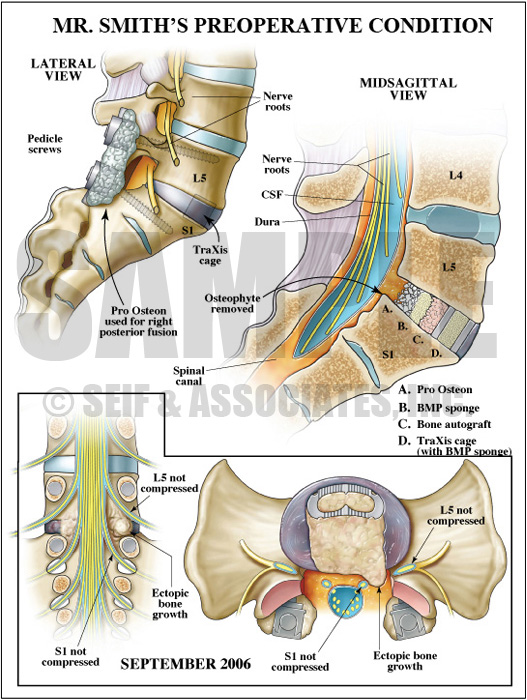
Next, the defense visual strategy tackled the development of the ectopic bone growth in the plaintiff’s spinal canal. This exhibit first showed the plaintiff’s initial post-operative condition, showing the placement of Pro Osteon, BMP sponge, Bone autograft, and the TraXis cage with BMP sponge in order to show that at the conclusion of the procedure, there was no graft material in the spinal canal and neither the L5 nor the S1 nerve roots were compressed. An overlay showed that by several months after the procedure, the ectopic bone growth was extruding into the spinal canal, but it was below and above the L5 and S1 nerve roots, respectively, and not compressing either root.
Exhibit 5 depicts the patient’s preoperative condition.
Overlay showing bone growth extruding into the spinal canal.
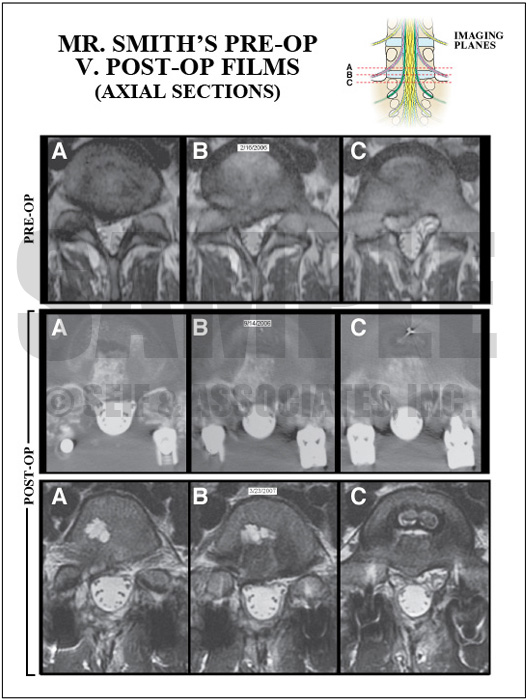
Lastly, in order to reinforce the defense contention that the post-operative condition showed no impingement on either the L5 or the S1 nerve roots on the right, the next exhibit showed the jury the pre-operative films compared to the post-operative films, using overlays to explain what is seen on these films.
Exhibit 6 depicts the patient’s radiological postoperative films.
Interpretative overlay used in trial.
The visual exhibits created for this case served to simplify and clearly outline the defense’s case in the setting of complex anatomy, pathology, and surgical technique, and were instrumental in obtaining a defense verdict.
—Editorial contributed by Emily Ullo Steigler, MS, CMI
—Illustrations contributed by Robert Edwards, MS, CMI